A Comprehensive Guide to Peritoneal Dialysis

Peritoneal dialysis (PD) is a treatment option for individuals with end-stage renal disease (ESRD), offering flexibility and independence compared to hemodialysis. Understanding the principles, procedures, benefits, and considerations of peritoneal dialysis is important for patients, caregivers, and healthcare professionals.
Continue reading as we explore the details of
peritoneal dialysis to provide a professional overview.
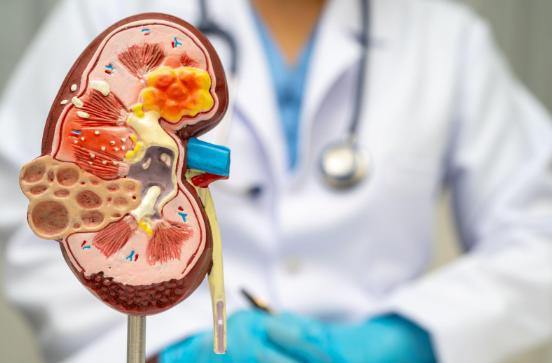
Understanding Peritoneal Dialysis
Peritoneal dialysis is a renal replacement therapy that utilizes the peritoneal membrane, a natural filtration barrier within the abdominal cavity. A sterile dialysis solution, rich in electrolytes and glucose, is introduced into the peritoneal cavity through a catheter. Dialysis removes metabolic waste products and extra fluid from the body by diffusing through the peritoneal membrane, removing toxins, and restoring electrolytes.
When Do You Need Peritoneal Dialysis?
If your kidneys can no longer function properly, you need dialysis. Kidney damage frequently worsens over many years as a result of conditions like:
- Diabetes mellitus
- High blood pressure
- A class of illnesses known as glomerulonephritis inflicts damage to the kidney's blood-filtering tissue
- Genetic diseases, including one called polycystic kidney disease, cause many cysts to form in the kidneys
- Prolonged use of medications like pain relievers that may harm the kidneys
Types of Peritoneal Dialysis
Peritoneal dialysis (PD) offers two main modalities, each with distinct features and benefits tailored to individual patient needs: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD).
Continuous Ambulatory Peritoneal Dialysis (CAPD)
CAPD is the most common form of peritoneal dialysis, allowing patients to exchange dialysis solutions throughout the day manually.
Here's how CAPD works:
- Manual Exchanges: Patients perform several dialysis solution exchanges daily, typically four to five times, depending on the prescribed regimen.
- Flexibility: CAPD provides patients with flexibility and independence as they can carry out exchanges at home, work, or during travel without requiring specialized machinery.
- Mobility: Since CAPD does not require a cycler, patients can move around during exchanges, enhancing their quality of life.
- Continuous Clearance: With regular exchanges, CAPD ensures continuous clearance of metabolic waste products and excess fluids, helping maintain optimal fluid balance and electrolyte levels.
Automated Peritoneal Dialysis (APD)
APD utilizes a cycler machine to perform dialysis exchanges automatically while the patient sleeps. Here are the key features of APD:
- Cycler-Assisted Exchanges: Patients connect to a cycler machine at night, which performs a series of automated exchanges using pre-programmed settings.
- Overnight Treatment: APD allows patients to undergo dialysis while they sleep, minimizing disruptions to daily activities and promoting restful sleep.
- Convenience: The automated nature of APD reduces the burden of manual exchanges during the day, offering convenience and ease of use for patients and caregivers.
- Tailored Therapy: Customizing APD to individual patient needs is possible, with adjustments to dwell times, fill volumes, and exchange frequencies to optimize dialysis adequacy.
Procedure and Technique
The procedure for peritoneal dialysis involves several key steps:
Catheter Insertion
It involves implanting a flexible, soft catheter into the abdominal cavity, which allows access to dialysis solutions.
Dialysis Solution Exchange
Using a sterile technique, the patient connects the catheter to drainage and infusion lines to perform exchanges, following prescribed schedules and volumes.
Monitoring and Complications
Regular fluid balance, blood pressure, and dialysis adequacy monitoring are essential. It is imperative to promptly address complications such as fluid imbalances, catheter malfunctions, and peritonitis.
The Benefits of Peritoneal Dialysis
In the US, kidney failure affects approximately 750,000 people annually. Peritoneal dialysis (PD) presents a range of advantages for patients with end-stage renal disease (ESRD) compared to other forms of dialysis. Including the following:
Flexibility and Independence
Unlike hemodialysis, which requires patients to visit a dialysis center multiple times per week for several hours each session, peritoneal dialysis allows patients to perform treatments at home or other convenient locations. This flexibility enables patients to maintain their daily routines, continue working, and travel more easily, promoting independence and normalcy.
Preservation of Residual Kidney Function
Peritoneal dialysis helps preserve residual kidney function in patients with ESRD better than hemodialysis. Preserving residual kidney function is associated with better clinical outcomes, including improved survival rates, reduced cardiovascular risk, and enhanced quality of life. By maintaining residual kidney function, peritoneal dialysis may delay the progression of kidney disease and decrease the need for additional interventions such as kidney transplantation.
Lower Healthcare Costs
Because patients can perform treatments at home without needing expensive dialysis equipment or frequent clinic visits, peritoneal dialysis reduces the financial burden on healthcare systems and payers. Additionally, the reduced need for transportation to dialysis centers and the potential complications associated with hemodialysis can result in overall cost savings for patients and healthcare providers.
Better Hemodynamic Stability
Peritoneal dialysis offers more gradual fluid and solute removal than hemodialysis. This helps with better hemodynamic stability and fewer fluctuations in blood pressure during treatment. By maintaining hemodynamic stability, peritoneal dialysis helps minimize the risk of cardiovascular events and enhances overall patient comfort and well-being.
Home-Based Care and Patient Empowerment
Peritoneal dialysis empowers patients to take an active role in managing their care and treatment. Through comprehensive training and education, patients and their caregivers learn to perform peritoneal dialysis exchanges, monitor their health status, and recognize signs of potential complications. This sense of empowerment fosters greater patient engagement, adherence to treatment regimens, and improved clinical outcomes over the long term.
Final Thoughts
Peritoneal dialysis provides a platform for patients, caregivers, and healthcare professionals to make well-informed decisions. A thorough grasp of the principles, procedures, benefits, and challenges associated with peritoneal dialysis improves patient outcomes. Additionally, by offering patients suitable education, support, and oversight, peritoneal dialysis enhances their quality of life and empowers them to manage their kidney health effectively.
Metropolitan Kidney Center offers compassionate support and expertise for those seeking comprehensive renal care and considering peritoneal dialysis as a treatment option. Our team helps empower patients with the knowledge and resources needed to make informed decisions about their health journey.
Schedule a visit with us today.